Acupuncture
Acupuncture in Santa Monica

Acupuncture is more than 5,000 years old, based on an energy systems model rather than a biomedical model of healing.
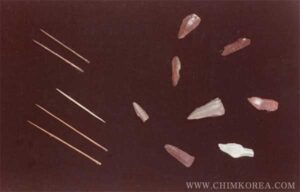
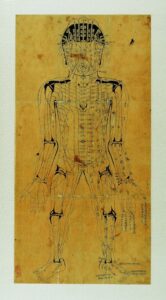
Acupuncture is based on the concept that our bodies contain energy, a vital life force that gives us our ability to move, think and feel. This life force, known as Qi (pronounced “chee”) runs through pathways in the body called Meridians, which have been determined after centuries of observation.
The Origin and History of Acupuncture
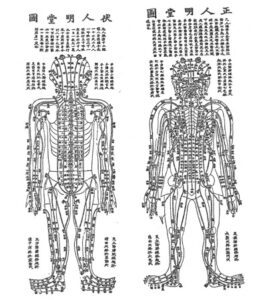
In Emperor’s Classic of Internal Medicine, huangdi neijing suwen(202-220 AD),which is the bible of the traditional Chinese medicine, We find the word, ‘bianshi’.
“故東方之域 天地之所始生也 魚鹽之地 海濱傍水 其民食魚而嗜鹹 皆安其處 美其食”
The eastern land, where Tiandi (the World) originated, produces fish and salt. People around the sea eat fish and salty food, which is very comfortable place and people have good food.
“魚者使人熱中 鹽者勝血 故其民皆黑色疎理其病皆爲癰瘍 其治宜砭石 故砭石者 亦從東方來”
Fish generates heat in the body and salt does harm to blood, people are dark-skinned and pores bigger and when they have boils, they should be treated by Bianshi. Therefore bianshi originated from the East.
The practice of acupuncture can perhaps be traced as far back as the Stone Age, with the Bianshi, or sharpened stones. Stone acupuncture needles in different size and shapes dating back to 3000 B.C. have been found by archeologists in Inner Mongolia, Hamkyong Province, Northern Korea and Shandong province, China, which were used to cut boils and drain the pus.
And during hunting and warring, people got injured often and they needed to stop the pain and bleeding by pressing and rubbing with a piece of stone, bone, arrow head. Along the course of many repeated experience, they found the empirical therapeutic points which is today called acupuncture points.
After Spring and Autumn Period and Warring States Period(around 200 BCE), these bianshi started to be replaced with iron needles called Jiu zhen(nine iron needles) used for different purposes and more systematically and many acupuncture books published.
Today, acupuncturists use the disposable stainless steel needle hair thin and flexible, which is called haozhen(hair needle), one of the old nine needles in its shape.
Introduction of Acupuncture to the US
In the 1970s, acupuncture became better known in the United States after an article appeared in ‘The New York Times’ by James Reston, who underwent an emergency appendectomy while visiting China. While standard anesthesia was used for the actual surgery, Mr. Reston was treated with acupuncture for post-operative discomfort. The National Acupuncture Association (NAA), the first national association of acupuncture in the US, introduced acupuncture to the West through seminars and research presentations.
The origin of the word ‘zhen’ – Acupuncture
The origin of the word zhen ‘鍼’ evolved from bian shi 砭石to zhen shi 箴石, and to zhen鍼
箴(zhen)=竹(zhu/bamboo)+咸(shian/fall, drop)
鍼(zhen)=金(jin/metal)+ 咸(shian/fall, drop)
Today we call acupuncture Zhenjiu 鍼灸, which in fact refers to acupuncture together with moxibustion.
Eastern Medicine consists of three major modalities: First is zhen-acupuncture, second jiu-moxibustion and the last yao-herbs. Therefore ‘zhen’, acupuncture has the most important role in Eastern Medicine.
The Effect of Acupuncture
- Regulate qi and flow it harmoniously
- Lower the temperature by which it treats the infection
- Relieve the pain
- Regulate the Autonomic nervous system
- Strengthen the immune system and prevent disease
How Acupuncture Works?
Acupuncture is thought to act on meridians. In the form of the treatment most widely practiced in the U.S., hair-thin needles are inserted into the skin at specific points along the meridians to redirect or unblock stagnant qi. These so-called acupoints correspond to different organs or systems in the body.
For example, inserting a needle at a point inside the forearem known as PC6 is intended to treat nausea; needling lv3, on top of the foot, is meant to help with motor function.
Studies suggest that inserting needles into acupoints does affect the body, and in potentially meaningful ways. In a study of 37 subjects published this year in the journal Neuroscience letters, inserting a needle into acupoint LI4 on the hand-traditionally used to treat pain-was shown to deactivate parts of the brain that are involved in processing pain.
Indeed, a decade of acupuncture imaging research has shown that “people who get better with acupuncture have clear changes in their brain function,” says dr. John Farrar, a pain researcher at the university of Pennsylvania School of Medicine. Changes are seen in the thalamus, a brain region that processes information from the sense, including touch and also pain.
But acupuncture also affects activity in the brain region called the cingulated gyrus as well as other brain structures that make up the limbic system, which processes the range of human emotions and memory.
The fact that acupuncture deactivates the brain’s limbic system suggests it “diminishes the emotional part of the pain experience.”
Hormone release could be a key to such brain changes. Thirty years ago, about the same time acupuncture started to pique the interest of Americans, Chinese medical researchers began studying it in animals. They showed-and subsequently western researchers confirmed- that acupuncture increased the body’s production of its own natural painkillers, known as endogenous opioids, or endorphins. People experienced no pain relief from acupuncture if they were first injected with a drug that blocked the opioids’ activity.
Today most western researchers agree that acupuncture’s stimulation of endorphins plays a big part in explaining how the practice works.
The WHO, the National Center for Complementary and Alternative Medicine (NCCAM) of the National Institutes of Health (NIH), the American Medical Association (AMA) and various government reports have studied and commented on the efficacy of acupuncture. There is general agreement that acupuncture is safe when administered by well-trained practitioners using sterile needles, and that further research is appropriate.
What symptoms can be effectively treated by Acupuncture?
In 2003, the World Health Organization(WHO) published a review and analysis of controlled clinical trials on acupuncture. They listed the following as “Diseases, symptoms or conditions for which acupuncture has been proved – through controlled trials – to be an effective treatment”
If you live in Santa Monica or the Los Angeles area, Tao of Medicine and Dr Hoon Kim can provide Acupuncture to successfully treat the following in a holistic and natural way:
- Allergic rhinitis (including hay fever)
- Biliary colic
- Depression (including depressive neurosis and depression following stroke)
- Dysentery, acute bacillary
- Dysmenorrhoea, primary
- Epigastralgia, acute (in peptic ulcer, acute and chronic gastritis, and gastrospasm)
- Facial pain (including craniomandibular disorders)
- Headache
- Hypertension, essential
- Hypotension, primary
- Induction of labor
- Knee pain
- Leukopenia
- Lower back pain
- Malposition of fetus
- Morning sickness
- Nausea and vomiting
- Neck pain
- Pain in dentistry (including dental pain and temporomandibular dysfunction)
- Periarthritis of shoulder
- Postoperative pain
- Renal colic
- Rheumatoid arthritis
- Sciatica
- Sprain
- Stroke
- Tennis elbow
What is Meridian?
Meridians form a network of energy pathways that are connected to different organs in the body. Along these meridians are points that can be accessed. There are hundreds such points on the body.
The needles help the energy flow well; it’s like reprogramming the body’s computer.
When the needles enter the point of access, they move the energy, helping to increase circulation throughout the meridian, which leads to an overall balance of one’s qi throughout the whole body. Ultimately, a balanced qi leads to improved physical, mental and emotional health.
The Researches of The Meridian Theory and Mechanisms of Acupuncture
For thousands of years, acupuncture has been based on the premise that specific points along the meridians correspond to specific organs, such as liver, and functions, such as the motor control. From the 1970’s and 90’, the relationship between acupoints and their related organs was a key focus of acupuncture research.
The meridians depicted in Chinese medical charts have no obvious anatomical basis-though diagrams of them do bring the nervous system to mind.
Meridians and acupoints might also correspond to areas of the body with physiologically distinct properties. In a study published in the scientific journal anatomical record in 2002, Dr. Helene Langevin, an associate professor of neurology at the University of Vermont College of Medicine, showed that about 80% of the acupoints o the arm correspond to areas of connective tissue between muscles.
Langevin is now examining what implications this might have for how acupuncture sends messages to the brain. She has published data showing that when needles are inserted into acupoints, the underlying connective tissue winds around the needle “like spaghetti around a fork,”she says. This doesn’t happen when a needle goes into a non-acupuncture points.
Langevin has also shown that the winding action causes the cells in the area to change shape, a process that she theorizes might signal the central nervous system. She is testing the theory in a series of animal experiments.
Other, older studies conducted and published in Asia and Europe during the 1970’s and ‘80s produced evidence suggesting that acupoints might be areas of very low electrical resistance, might be slightly more sensitive to touch or might lie near major nerve pathways. But scientists don’t know the significance of these characteristics.
Evidence from Neuroimaging Studies
In more recent years, brain imaging has been used to clarify the relationship between acupoints and the functions they represent. The practice way pioneered by Zhang-hee Cho, UC Irvine professor of radiological sciences.
Cho showed in a series of imaging experiments, published in 1998 in the proceedings of the national academics of sciences, that needling several acupoints for eye problems-located near the little toe-in a group of 12 volunteers increased activity in the visual cortex, the part of the brain governing vision.
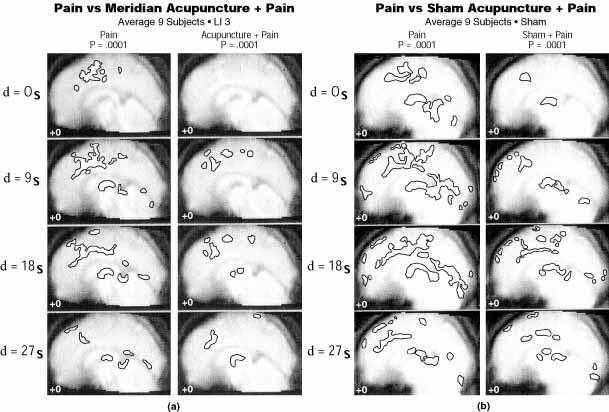
Figure 8. Side-by-side comparison of 2 cortical activations seen at the mid-line sagittal view due to: (a) pain vs meridian acupuncture (LI 3) + pain stimulation and (b) pain vs sham acupuncture + pain stimulation, respectively. Decreases in activation of the 2 appear similar, suggesting that they are based on similar neural mechanisms.
Yet when Cho and his colleagues stimulated random points, located a few centimeters away from each point, no activity occurred in the visual cortex.
Dr. Randy Gollub, assistant director of psychiatric neuro-imaging at Massachusetts General Hospital, is also investigating the differences in brain activity generated by needling at real and fake acupoints. In an ongoing study, healthy volunteers are subjected to pain and then given either real or sham acupuncture. So far, both treatments appear to activate or deactivate various regions of the brain involved in controlling the body’s reaction to pain: “they’re a lot more alike than they are different,” Gollub says.
But, she adds, it looks as if the brain’s response is stronger for true acupoints than for sham ones. “think of it as a mountain range, with the acupuncture points as peaks, as long as you’re not in the valley, the acupuncture is probably going to have some effect.”
Cho, for one, has found in recent studies that inserting needles in real or sham sites produces similar changes in parts of the brain perceiving pain.
In simplified terms, he thinks that inserting a needle at almost any point on the body triggers a series of biochemical messages between the brain’s hypothalamus and the hormone-producing pituitary and adrenal glands. The signals tell the body to alter its production of, for example, certain stress with stressors – such as bacteria, viruses, emotional trauma or pain.
In fact, cho believes that acupuncture might someday be refined to the point where the use of a dozen or more needles could be traded in for a single well-placed needle. “one good stimulation may be enough” for lasting pain relief, he says.
Gate-control Theory of Pain
The “gate control theory of pain” proposed that pain perception is not simply a direct result of activating pain fibers, but modulated by interplay between excitation and inhibition of the pain pathways. According to the theory, the “gating of pain” is controlled by the inhibitory action on the pain pathways. That is, the perception of pain can be altered (gated on or off) by a number of means physiologically, psychologically and pharmacological. The gate-control theory was developed in neuroscience independent of acupuncture, which later was proposed as a mechanism to account for the hypothesized analgesic action of acupuncture in the brain stem reticular formation in 1976.
This leads to the theory of central control of pain gating, i.e., pain blockade at the brain (i.e., central to the brain rather than at the spinal cord or periphery) via the release of endogenous opioid (natural pain killers in the brain) neurohormones, such as endorphins and enkephalins (naturally occurring morphines).
Neurohormonal Theory
Pain transmission can also be modulated at many other levels in the brain along the pain pathways, including the periaqueductal gray thalamus, and the feedback pathways from the cerebral cortex back to the thalamus. Pain blockade at these brain locations is often mediated by neurohormones, especially those that bind to the opioid receptors (pain-blockade site).
Some studies suggest that the analgesic (pain-killing) action of acupuncture is associated with the release of natural endorphins in the brain. This effect can be inferred by blocking the action of endorphins (or morphine) using a drug called naloxone. When naloxone is administered to the patient, the analgesic effects of morphine can be reversed, causing the patient to feel pain again. When naloxone is administered to an acupuncture patient, the analgesic effect of acupuncture can also be reversed, causing the patient to report an increased level of pain. It should be noted, however, that studies using similar procedures, including the administration of naloxone, have suggested a role of endogenous opioids in the placebo response, demonstrating that this response is not unique to acupuncture.
One study performed on monkeys by recording the neural activity directly in the thalamus of the brain indicated that acupuncture’s analgesic effect lasted more than an hour. Furthermore, there is a large overlap between the nervous system and acupuncture trigger points (points of maximum tenderness) in myofascial pain syndrome.
Evidence suggests that the sites of action of analgesia associated with acupuncture include the thalamus using fMRI (functional magnetic resonance imaging) and PET (positron emission tomography) brain imaging techniques, and via the feedback pathway from the cerebral cortex using electrophysiological recording of the nerve impulses of neurons directly in the cortex, which shows inhibitory action when acupuncture stimulus is applied. Similar effects have been observed in association with the placebo response. One study using fMRI found that placebo analgesia was associated with decreased activity in the thalamus, insula and anterior cingulate cortex.
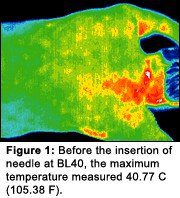
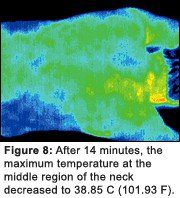
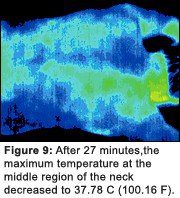
The Study with Thermography using the infrared images by Yin Lo, Ph.D.
The left picture is the before acupunctuer, the red color region means the pain or inflammed, the picture 9 doesn’t show the red region, pain or inflammation significanlty decreased after acupuncture treatment.
Recently, acupuncture has been shown to increase the nitric oxide levels in treated regions, resulting in increased local blood circulation. Effects on local inflammation and ischemia have also been reported.
Acupuncture Treatment Time (Needle Retention Time) – How long you have needles on the body.
There have been people asking me of the needle retention time or actual treatment time. Some seem to believe that the longer is the better in having needles on the body, some want to know why I give the different duration for each different condition and so on.
Then why some acupuncturists give longer time (some longer than 30 min, even 1 hour) and some shorter(10min)?
Theoretical Background for Specific Duration Times: 1.15-20 minutes : The Nan Jing-The Classic of Difficulties, Chapter 23.
According to The Nan Jing , Qi and Blood move through the meridians at the rate of six cun* for each complete inhalation and exhalation. The total length of the Meridians and Collaterals equals 1620 cun. 1620 divided by 6 equals 270, so it is said that 270 breaths are required for Qi to make one complete cycle through the body. However, this number could vary based on a person’s breath rate. If a person breathes 14 times/minute, it will take 20 minutes (270/14) for Qi to make a complete cycle. If a person breathes 18 times/minute, only 15 minutes (270/18) will be needed for Qi to make the complete cycle. Therefore needle retention time can be calculated around 15-20 minutes. *Cun is a Chinese proportional unit of length
2. 30min: The Ling Shu-Spiritual Pivot, Chapters 15 & 18
the Qi and Blood circulated through the channels 50 times per day. Since 24 hours equals 1440 minutes, dividing 1440 by 50, we get the 28 minutes and 48 seconds. This is where we get the guideline for approximately 30 minutes of needle retention time.
How long is the right time for having needle in a session?
Some renowned acupuncturists put the needle over less than 5 locations and stimulate intensely and when they see the positive effect as expected, those needles are taken off or stay less than 5 minute.
They claim that once your brain picks up the signal from the needle and starts secreting the neurotransmitter for the pain relief or whatsoever and your patients show the improvement, you don’t really have to leave the needles any more.
Some practitioners report that the best results where achieved after 45 minutes of retaining the needles. Master Tung style acupuncture also used needle retention of 45 minutes, in which he stimulated the points every 15 minutes. Some Korean acupuncturist who does Korean taoistic technique gives 1hr- 2hr needle retention to balance the whole body Qi.
So many factors are there to choose the right acupuncture time; each patient’s condition or the different season or even weather condition or the specific acupuncture technique that your acupuncturist performs. Therefore I strongly believe that choosing the right time is solely up to your acupuncturist’s differentiation, diagnosis and treatment plan for the best results and what kind of acupuncture technique he or she performs.
Resources: